Treatment - Chemotherapy
QOL Tree
Treatment
Before Treatment
Ceremony
Surgery
Radiation
Chemotherapy
After Treatment
Palliative Care
Hospice and EOL
Chemotherapy
- History of Chemotherapy
- Mustard gas, a poison, was used in World War I (1914). The soldiers who had cancer and were exposed to the gas showed improvement in their cancers. These healing effects of mustard gas were discovered by accident and called “chemotherapy”
- Many changes have occurred in chemo
- The types of drugs used
- How the drugs are given to the patient
- Intravenous [IV, injected in a vein]
- Orally [pills, by mouth]
- Catheter [through a tube sewn into the body when the veins cannot handle the drugs or when the amount of drugs is very large]
- The strength of the drugs [dosage]
- The combinations of drugs
- How often chemo is given [frequency]
- How long the series of chemo treatments last (6 weeks, then a break for a few months) [duration]
- Prior to the 1950s, treatment for the majority of cancers was limited to either surgery or the use of radiation
Chemotherapy today
- There are more than 100 different chemotherapy drugs
- The discovery of the use of methotrexate in curing a rare cancer marked the first time a cancer had been cured
- This led to the development of many of today’s common cancer treatments
- The drugs are used in different proportions or amounts
- The drugs are combined with other chemo drugs (chemo cocktail)
- The amount and type of chemo you receive is based on the
- The type of cancer cells (histology)
- The size of your tumor
- Whether or not your cancer has spread (metastasized)
How chemo works
- Cancer cells grow and duplicate quickly.
- Chemo uses drugs that kill cells or slow down their duplication.
- In general, chemotherapy drugs affect the DNA of the cells by interfering with cell duplication.
- Chemo drugs are poisons that breaks up the DNA so that it cannot make new cells
Why both cancer and healthy body cells are affected by chemo
- Chemo drugs affect the DNA of both the cancerous and healthy cells
- The healthy cells that are particularly susceptible to chemo are by cells that multiply quickly:
- The skin (including body, facial, and head hair)
- The digestive system (gastrointestinal tract)
- The bone marrow (that makes red and white blood cells)
Goals of chemotherapy
- Cure
- Control - extend length and quality of life when hope of cure is not realistic
- Palliation – ease symptoms/ improve comfort
Purpose(s) for Chemotherapy
- Shrink the size of a tumor before surgery or radiation
- Kill or poison cancer cells when surgery is not an option (to destroy or slow the growth of cancer cells)
- Kill or poison any remaining cancer cells that were not removed during surgery (to stop cancer from spreading)
- Relieve cancer pain or other symptoms
Why you may receive a different combination and dosage of chemo drugs than the patient sitting next to you
- The most common reason is because your cancer is different from the patient sitting next to you (you have a different type of breast cancer)
- Another reason is that you may have had severe side effects and they are using a different combination of drugs (cocktail) to see if you react better to the treatment
- Another reason is that one of you may be on a clinical trial that is using a drug combination that may or may not be better than standard treatment for your type of cancer.
Chemotherapy is the treatment of choice for:
- Leukemias, lymphomas (blood forming cells)
- Solid tumors that have metastasized
- Cancers with high potential of spread/ recurrence
How does it work?
- Attack cells when they are dividing (cancer cells divide much more often than do normal, healthy cells)
- Damage genetic material inside the cell that allows the cell to divide and reproduce
- Block chemicals that the cell needs to enable it to divide and reproduce
Types of chemotherapy
- Standard therapies used alone or in combination with newer therapies and other treatments
- Alkylating agents
- Interferes with DNA replication (cross link DNA strands) and inhibits cancer cell growth
- Most agents are cell cycle nonspecific
- Such as: Busulfan (Myleran), Cyclophosphamide, Temozolamide (Temodar)
- Antimetabolites
- Drugs that interfere with one or more enzymes or their reactions that are necessary for DNA synthesis.
- They affect DNA synthesis by acting as a substitute to the actual metabolites that would be used in the normal metabolism
- Inhibit protein synthesis, substitute metabolites, or structural analogues during DNA synthesis and inhibit DNA synthesis
- For example, antifolates interfere with the use of folic acid
- Most are cell cycle/phase specific
- Such as: 5-fluorouracil (5-FU), 6-mercaptopurine (6-MP), Capecitabine (Xeloda), Gemcitabine)
- Anti-tumor antibiotics
- A type of anticancer drug that blocks cell growth by interfering with DNA, the genetic material in cells
- Interferes with nucleic acid synthesis and function. Inhibit RNA synthesis
- Also called anticancer antibiotic and antineoplastic antibiotic
- Most agents are cell cycle nonspecific
- Such as: Dactinomycin (Cosmegen), Bleomycin, Daunorubicin (Cerubidine, Rubidomycin) and Doxorubicin (Adriamycin PFS, Adriamycin RDF)
- Topoisomerase inhibitors
- Enzymes that participate in the overwinding or underwinding of DNA. ... In order to prevent and correct these types of topological problems caused by the double helix
- Chemical compounds that block the action of topoisomerases (topoisomerase I and II), which are enzymes that control the changes in DNA structure by catalyzing the breaking and rejoining of the phosphodiester backbone of DNA strands during the normal cell cycle
- Such as: Etoposide, Irinotecan (Camptosar), Topotecan (Hycamtin)
- Mitotic inhibitors
- A type of drug that blocks cell growth by stopping mitosis (cell division); also called antimitotic agent
- Bind with microtubular proteins, crystallize the mitotic spindle, and result in metaphase arrest
- Phase cycle specific
- Such as: Docetaxel (Taxotere), Eribulin (Halaven), Ixabepilone (Ixempra), Paclitaxel (Taxol), Vinblastine
Methods of Administration
- Oral
- Intravenous (IV)
- Catheter, port, pump
- You sit in a room alone or with other patients who are also getting chemo
- Your family or friends can come sit with you while you receive the treatments
- You may want to bring a blanket because if your treatment lasts for a few hours, you may get cold (the liquid in the IV is cold)
- You may want to have a glass with some ice chips to suck on
- You may want to drink a mild tea, like ginger tea to help reduce the upset stomach
- If you are diabetic, you need to bring a healthy snack or drink so that your blood sugar doesn’t get too low while you are in treatment
- Injection
- Intrathecal
- Intraperitoneal (IP)
- Intra-arterial (IA)
- Topical
Classifications of Chemotherapy
- Cell cycle specific agents (phase specific)
- Major effects exerted only when cells in a specific part of the cell cycle
- Cell cycle nonspecific agents
- Effects are exerted on cells at any phase
The Cell Cycle and Phase-Specific Chemo
- Many chemotherapy drugs are designed to attack the cells during a specific phase of cell reproduction, such as:
- One drug may target the cell ONLY during the G1 phase
- Another drug may target the cell ONLY during the S phase
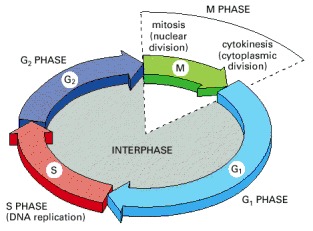
Reference: https://www.ncbi.nlm.nih.gov/books/NBK26869/figure/A3171/?report=objectonly
- Cell Phase:
- G1 phase (pre DNA) 8-48 hrs
- RNA and protein synthesis actively preparing for DNA synthesis
- S phase (DNA synthesis) 10-30 hrs
- DNA doubles in preparation for mitosis
- G2 phase (pre-mitotic phase) 1-12 hrs
- DNA synthesis discontinues and prepares for cell division
- M phase (mitosis) 1 hr
- Spindle formation, separation of chromosomes and cell division
- G0 phase (resting phase)
- Cell is no longer dividing and highly resistant to chemotherapy during this phase
- G1 phase (pre DNA) 8-48 hrs