Side Effects - Sexuality & Intimacy
Sexuality and Intimacy Branch withing the NACES Quality of Life Tree
The Author of this Branch is Linda U. Krebs, RN, PhD, AOCN, FAAN
Welcome to the sexuality and intimacy branch!
The purpose is to help with any problems you may have due to changes in sexual feelings and responses caused by your cancer or cancer treatment
- Cancer and its treatment can affect your sexuality and your relationships with others
- This branch will help you understand some of the possible changes and give you some ideas about what you can do to
- Improve your sexual functioning and your relationships during and after cancer treatment
What is sexuality?
- Sexuality is more than just sex
- Sexuality includes:
- Feeling attractive and liking the way we look (body image)
- Being able to feel loved or be loving and enjoying touching or caressing
- Being able to have children if desired
- Sexuality is a person's view of himself or herself as an attractive person who can gain the attention and affection of others
- Sexuality is a part of every area of our lives
- it is part of the way we relate to others
- it is what we believe and how we behave
- our views are affected by many things and vary over our lives
- Sexuality is very personal and is different for each person
- Sexuality is influenced by many things including religion, culture, age and situation
- Your sexuality may be changed by life events such as marriage, illness, money difficulties or where you live
- We show our sexuality by what we wear, how we walk or move and in who we have sex with
- "Normal" sexual relations are whatever is comfortable for you and your partner (if you have one)
- It is normal for people with cancer to lose interest in sex at times
- It is also normal to be interested in sex throughout your life
- While many believe that sex is only for the young, many are interested in sex throughout their lives
What is body image?
- Body image is the way you see yourself (fat, thin, pretty) as well as how you think others see you
- Body image is the mental picture you have of what you look like
- This image may or may not be real (the teenaged girl with an eating disorder may see herself as fat even though she only weights 90 pounds)
- Our body image changes throughout our lifetime, whether or not we have cancer or get cancer treatment
- Your body image may be affected by changes in your body's appearance due to:
- Weight loss or gain
- Hair loss (alopecia [al-o-pea-sea-ah])
- Mouth sores (mucositis [mew-co-sigh-tis])
- Extreme tiredness (fatigue)
- Other changes that may or may not be seen by another ( a scar, loss of a breast)
How common are sexual problems for cancer survivors?
- Problems with sexual function, intimacy or the ability to have children in the future are common in people during and following cancer treatment
- Sexual problems occur in:
- About half (50%) of women who have breast cancer
- About half (50%) of those with gynecological [guy-neh-co-loge-ih-cal] cancer (cancer of the ovaries, cervix, and womb)
- Almost three-fourths (70%) of men with prostate cancer will have some problems
- Problems can affect your desire for sex, your ability to be aroused or your pleasure in sexual activities
- These problems can be severe and often last a long time.
- Sometimes other side effects will improve while problems with your sexuality will continue
What are the common sexual problems seen in those with cancer?
- Loss of desire for sex (men and women)
- Not able to have an erection
- Pain with sex (women)
- Trouble reaching orgasm (men and women)
- Changes in body image due to such things as removal of body parts such as your breast, scars, weight changes, swelling of your arm(s) or leg(s) due to lymph node removal (lymphedema) and hair loss (alopecia)
- Difficulty touching or being touched
- Problems talking about sexual needs
- Not being able to become pregnant or father a child
- Stress in relationships with sexual partners
Who is at risk for sexuality problems?
Some people with cancer are more likely to have problems with sexuality than others. Those at higher risk are:
- Women
- Being 30 years of age or older
- Having surgery such as a hysterectomy [hiss-ter-ec-toe-me] for a gynecologic cancer
- Men
- Being older than 15 years of age
- Having surgery to the testicles or prostate
- Women and Men
- Getting chemotherapy or radiation therapy
- Getting radiation treatments to your abdomen (ab-dough-men)
- Having surgery to your abdomen, breast and/or the head and neck area
- Taking medications such as drugs to treat depression, high blood pressure, pain, nausea or anxiety
- Having untreated side effects such as fatigue, mouth sores or pain
- Feeling emotional (sad, angry, depressed) about having cancer, losing a body part, having hair loss and/or losing or gaining weight
- Having marital conflict or financial stress
- Having another illness such as diabetes, heart disease or arthritis
- Having poor health habits such as smoking, using alcohol or drugs
The Medicine Wheel: The Body: Sexuality and Intimacy's Impact on the Body
Jared, please insert the medicine wheel graphic here: NACES/MedicineWheel.png
This section lists some of the ways in which changes to our bodies can cause changes in our sexuality.
What are the female sex organs and sexually responsive body areas for women?
- Women's sexual organs are both inside and outside the body
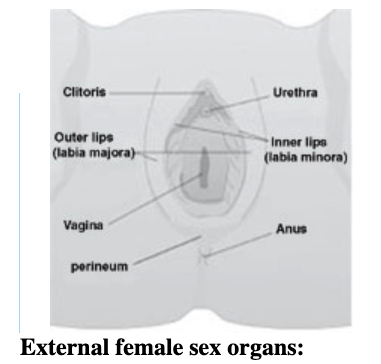
The organs outside the body include:
-
- The outer lips of the vagina, the labia majora [lay-bee-ah maa-jor-ah].
- When parted, these show the inner lips, the labia minora [lay-bee-ah mih-nor-ah].
- These lips join at the top to cover the clitoris [klit-er-iss]. The clitoris is the size of a pea and is usually sensitive to touch.
- Just below the clitoris is the opening for urine, the urethra [you-ree-thra].
- Below that is the opening to the vagina.
- Below that is the opening for stool, the anus [a-nus].
- The diamond shaped area of skin that includes the vagina and anus is called the perineum [pear-ih-knee-um].
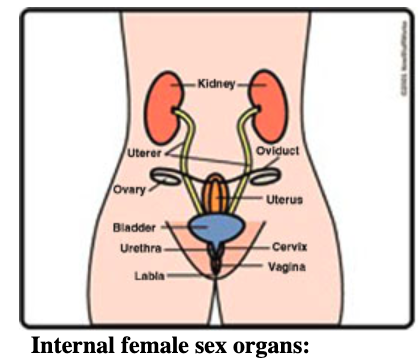
- Most of a woman's sex organs are inside the body.
- The organs inside the body include:
- The uterus (womb)
- The cervix [sir-vicks] (neck of the womb)
- The ovaries [oh-vah-rees]
- The fallopian [fah-low-pee-an] tubes
- The pelvis is the name given to the lower part of your abdomen
What are the other sexual areas on the body?
-
- The breasts and nipples
- Sensitive areas that respond to touch include:
- The back of the neck
- Behind the knees,
- The buttocks
- The inner thighs
- These areas may be different for each person
- These areas are called the erogenous [ee-rah-gin-us] zones.
What is sexual arousal?
-
- Sexual desire is used to describe an interest in sex. It is also known as libido [lih-bee-dough].
- Sexual desire can change with illness, pregnancy, during your monthly cycle or after the change of life (menopause).
- How you are feeling physically and emotionally also can affect your desire for sex.
What are the stages of sexual arousal?
-
- Your sexual response is made up of four stages or phases;
- Stage 1: Excitement or arousal
- This is the beginning of sexual feelings or feeling "turned on" and ready for sex.
- Physically:
- Your breathing and heart rate increase
- Your vagina becomes damp
- You may begin to sweat or your body may feel warmer
- These feelings can happen for many reasons such as being kissed, being touched or touching your partner or by a sexual fantasy.
- Arousal may, or may not, lead to orgasm.
- Stage 2: Plateau
- The body stays aroused
- The body is very sensitive to touch
- Stage 3: Orgasm
- This is also known as the sexual climax or "coming"
- Your body feels intense sensations that are like waves or contractions throughout the body
- Orgasm includes ejaculation [ee-jack-u-lay-shun] of sperm for men
- Stage 4: Resolution
- The body returns to its normal state
What can cause sexual desire and arousal to be less than usual?
-
- Sexual arousal can be less than usual if you are
- Very tired (fatigued)
- Feeling stressed
- Having pain
- Feeling anxious or depressed
- Using alcohol or drug excessively
- Having relationship problems
- Taking medicines for nausea, depression, heart problems, high blood pressure
- Feeling short of breath
- Feeling unhappy about your body
- Sexual arousal can be less than usual if you are
How can I increase my interest in sexual activities?
-
- Find things that usually lead to sexual desire and increase how often you do them
- Be as physically active as possible
- Do things that promote intimacy such as being close, cuddling, or having a romantic dinner
- Think about using sexual fantasies or materials
- Practice looking at your body. If you feel comfortable, touch your body as well (learn what feels good; what does not)
Effect of Cancer Treatment on Sexuality
How can cancer surgery affect my sexuality?
-
- Whether the changes in your sexuality are short term (temporary) or permanent (long term) will depend on the type of surgery you have.
- Surgery that removes the womb and ovaries will make you unable to have children (sterile/infertile) and may change how you function sexually.
- Surgery to the bladder or colon/rectum can damage nerves that affect how you respond to sexual activities and may decrease arousal
- Surgery to other areas of your body should not affect fertility, but may change sexual function because of changes in your body image or emotional concerns.
- Surgery to lymph nodes may cause swelling, pain and discomfort that affects sexual functioning
Label: CeCe Whitewolf, Confederated Tribes of Umatilla
Diagnosed 1998 with breast cancer

But what's happened and again no one tells me this and I and I try to ask the doctor to about this and he was old man and oh he must have been about 65 or 70. And I said because no one has explained to me about my insides and what it's like ya know what's in there? And I said well what have you done to me now, can I still have sexual intercourse? And what's going to happen? And he told me he said well I made you a cul-de-sac. I said, a cul-de-sac, what do you mean a culture sack? So he said he described it kind like he's made a little end, a circle end and that I'm cut off at the end like a culture sack and I said oh okay. Something's wrong though, the culture sack must not be, is not very long or something happened to the culture sack because what happens now is whenever Ron and I have sexual intercourse. I bleed every time, I ... It's like I have a menstrual cycle after we have our sexual intercourse. So something's wrong, and so I've got to go into the doctor and now I think I have to tell him that my culture sack is too short."
What kinds of surgeries can affect my sexuality?
- Hysterectomy [hiss-ter-ek-toe-me]
- Removal of the uterus (womb) and cervix .
- The upper end of the vagina is sewn shut after the womb and cervix are taken out.
- The vagina will be a little bit shorter (most women do not notice).
- While you are healing from surgery, your partner needs to be gentle.
- The normal time to wait to start having sex again is about 6 weeks after surgery (ask your provider for a definite length of time).
- Orgasm may feel a bit different since the nerves that make the clitoris respond to touch may be changed by your surgery.
- Oophorectomy [oo-four-ek-toe-me]
- Removal of the ovaries.
- Will cause menopausal (change of life) symptoms (hot flashes, mood swings) if both ovaries are removed.
- These symptoms start very soon after your surgery rather than happening slowly as happens with the normal change of life.
- See the section on menopause for more information about these symptoms.
- Mastectomy or lumpectomy
- Removal of all or part of the breast
- Mastectomy [mast-ek-toe-me] removes all of the breast tissue
- Lumpectomy [lump-ek-toe-me] removes part of the breast (the lump or area of the cancer and some surrounding tissue)
- Surgery to the breast can affect your sexuality if touching your breasts was part of your sexual arousal.
- Removing all or part of your breast can affect your body image. This may make you feel less womanly or attractive
- Making a new breast shape (breast reconstruction) at the time of mastectomy or even months later may decrease some of the sexual side effects of mastectomy
- Abdomino-perineal resection [ab-dom-in-oh pear-ih-knee-al ree-sec-shun]
- For cancers of the colon or rectum
- Nerves to the womb, cervix and clitoris may be changed by your surgery
- Sensations during sex and orgasm may not be the same as before your surgery.
- Vulvectomy [vuk-vek-toe-me]
- Simple vulvectomy removes the labia majora, labia minora and clitoris
- Radical vulvectomy removes all the above tissues, plus local skin and lymph nodes in your pelvis
- Sensations during sex will be changed
- Body image changes often affect your sexuality
- Creation of a Stoma [stow-mah]
- A stoma (opening) may be made if you have surgery to your bladder, kidneys, colon or rectum. A stoma also may be made if you are treated for advanced cervical or ovarian cancer
- When making a stoma, an opening is made in the skin of the abdominal wall to bring urine or stool out of the body (some may have an opening for stool and an opening for urine)
- The stoma is usually covered with a pouch to collect the stool or urine
- A stoma can make some lovemaking positions uncomfortable.
- Worry about the pouch leaking during lovemaking is common; emptying the pouch just before lovemaking will make this less likely
- Removal of lymph nodes
Can radiation therapy affect my sexuality?
Changes in sexuality and your ability to have children may be short term, last a long time but get better or may be permanent.
- Long term effects are most commonly due to:
- The total dose of radiation you get
- What part of the body is treated
- How long the treatment lasts (number of weeks)
- How old you are when you begin your radiation treatments
- Women closer to normal change of life will have fewer problems with menopause symptoms than those who are younger
- if you were able to have children before your radiation treatments
What kinds of changes in my sexuality can I expect?
- Radiation therapy to the pelvis can cause ovaries not to function as they should
- Your monthly cycle may stop
- You may have hot flashes and mood changes (see menopausal symptoms) Rick, please add link here
- You may not feel aroused or have normal lubrication in your vagina
- You may have diarrhea, sores in your vagina or be very fatigued
- The vagina may become narrower and less flexible after radiation therapy (see below for management)
- Radiation therapy to the breasts:
- May change how your breasts respond to touch or what clothing feels like on your skim
- May change the color and flexibility of the skin
- May affect sexuality through changes to body image
- Arousal may be affected if touching the breasts was a usual part of your sexual activities
Can I have sexual relations during radiation treatments?
- Unless you have bleeding or pain, you can usually have intercourse during your radiation treatments.
- Radiated skin may be very sensitive to touch
- Unless intercourse or touching is painful, you should still be able to reach orgasm if you could before your treatments.
- Ask your provider before using any lotions or creams on your irradiated skin
Can radiation therapy affect a pregnancy?
- Radiation treatments can damage an unborn baby
- You should be sure you are not pregnant before starting your treatments
- You need to use methods to prevent pregnancy during your treatment (condoms, birth control pills, etc.)
- If you are pregnant when you are diagnosed with cancer, sometimes the radiation treatments can be delayed until after the baby is born. Be sure to talk with your healthcare provider about this.
- You should not breast feed a baby from the breast that has been radiated. The possibility of breast infection is high. You can breast feed on the side that did not get radiation.
Can chemotherapy affect my sexuality?
- Depending on what type of chemotherapy you get, changes in sexuality may be short term, long term but eventually get better, or permanent.
- In general, sexual side effects are related to:
- Type of chemotherapy drug you get (some are more likely to cause sexual problems than others)
- Dose of each drug that you are given
- The total amount of time (in weeks or months) that you are treated with chemotherapy
- How old you are (the closer you are to normal change of life, the less likely you are to have problems with menopausal side effects)
- How long ago you finished chemotherapy (a longer time may be enough for your monthly cycles to start again).
- If your chemotherapy includes more than one drug (two drugs will usually cause more problems than just one drug)
- The medications used to treat you for nausea, pain or other treatment side effects
- The most common side effects that may affect sexuality are:
- Loss of your monthly cycle
- Starting the change of life earlier than usual
- Less interest in sex
- Decreased or difficulty becoming aroused
Can hormonal therapy affect my sexuality?
- Hormonal therapies such as Tamoxifen, Zoladex, and other anti-estrogens are often used to treat cancer
- These drugs may affect your sexuality because they can cause:
- Vaginal soreness, dryness or discharge
- Changes in your interest in sex (may be less or more than is common for you)
- Irregular monthly cycles
- Hot flashes and other menopausal symptoms
- Acne on your face, neck, back or arms
- For men taking female hormones, breast may get larger
Can biologic therapy affect my sexuality?
- Many of the new cancer treatments include drugs that affect different body systems or pathways that allow normal (and cancerous) cells to grow and function. These drugs may or may not affect sexuality (not a lot is known about this yet).
- The most common side effects of these drugs that may affect sexuality are:
- Flu like symptoms (aches, muscle soreness, fever)
- Fatigue,
- Less vaginal lubrication
- Skin rash
- Decreased sexual desire
- Irregular or no monthly cycle
- Pelvic pain
- Body image changes
Can having a bone marrow or stem cell transplant affect sexuality?
- Bone marrow or stem cell transplants are done to treat some types of cancer such as leukemia or multiple myeloma
- These treatments are very intense and have many side effects,
- Common side effects that may affect sexuality include:
- Less interest in sex
- Narrowing of the vagina
- Less vaginal lubrication
- Pain during intercourse
- Body image changes
- Chronic fatigue
- Chronic diarrhea
Are there any other greatments that may affect my sexuality?
- Drugs used to manage cancer treatment side effects (pain or nausea) can affect sexual function such as:
- Less interest in sex
- Lowered ability to have an orgasm
- Drugs likely to affect sexuality include:
- Antidepressants (treat depressions)
- Anti-nausea drugs (prevent nausea and vomiting)
- Sedatives (help you to sleep)
- Tranquilizers (make you less anxious)
- Antihistamines (used to treat symptoms of allergies)
- Steroids (used to prevent nausea and treat some forms of cancer)
- Narcotics (used to treat pain)
What is premature or early menopause?
- Known as the end of your monthly cycles, the change of life or simply "the change", menopause normally occurs in most women in their late 40s to early 50s (but can occur earlier or later)
- If you have your ovaries removed or receive chemotherapy or radiation to the pelvis, you may go through menopause earlier than normal (premature menopause)
What causes early menopause in cancer patients?
- Normal aging
- Removal of the ovaries (oophorectomy) by surgery
- Cancer treatment (radiation therapy, chemotherapy)
- Lack of estrogen to body tissues
What happens if I do not have enough estrogen in my body?
- You will have hot flashes or flushes
- You may feel irritable or weepy
- You may have difficulty getting to sleep or staying asleep
- You may have muscle and joint pain
- Your vagina with not stay moist and flexible
- You will have increased wrinkling
- You may have increased weight gain and weight is hard to loose
What are hot flashes?
- Hot flashes or flushes are a sudden onset of an uncomfortable feeling of intense heat
- Along with the sensation of heat you may have sweating and skin flushing, usually in the face and chest
- A hot flash usually lasts about 3 to 5 minutes
- Recovery from the hot flash takes about 30 minutes
- Some women have 2 or3 hot flashes each day; some may have 30 to 40 hot flashes each day
What treatments may be helpful to manage hot flashes?
- There are many methods suggested for treating hot flashes.
- Among them are estrogens, some antidepressants, herbs and other complementary methods such as vitamins, yoga and acupuncture.
- Some may work for you and some may not.
- Always talk with your healthcare provider before taking any medicines, herbs or vitamins as they may interfere with your cancer treatment.
What are some ways to decrease hot flashes without medications?
- Wear loose clothing; use natural fibers and layer your clothing
- Avoid spicy foods, hot tea/coffee, and alcohol
- Try to lessen stress
- Exercise daily
- Keep your thermostat at < 70 during day and <65 at night
Why do I have pain during intercourse?
- Pain during intercourse can occur in those who have surgery or radiation therapy to the pelvis
- Pain may occur if you have less lubrication (dampness) in your vagina than is usual for you
- If you are not aroused when you have intercourse, you may have less lubrication
- Being afraid of having pain can cause less lubrication and cause the vagina to tighten, this causes pain which then increases your fear of having pain
Label: CeCe Whitewolf, Confederated Tribes of Umatilla
Diagnosed 1998 with breast cancer

"But the issue is vaginal dryness. They didn't tell us with our chemo with all of our drugs that we would have vaginal dryness. And I've always wondered what the heck is vaginal dryness. Well now I know when you have sexual activity, your body puts out kind of a lubrication so that as the penis enters the vaginal area it doesn't hurt. It's not dry like sandpaper, when you have vaginal dryness you don't have that lubrication anymore and so like right now my vaginal canal is dry and if Ron and I have sexual activity we have to use a lubricant. And I didn't know what they meant by using a lubricant, where in the world do I get a lubricant. What's that all about? I'm 55 years old. Nobody told me these kinds of things as when I was growing up so we've also learned that in addition to, we'll keep talking about the lubricant.
You go into the grocery store, you go into Fred Meyers or Safeway and you go to where they have the male condom places that's where they have those lubricants, it's like a they said it's a KY jelly or some kind of little squeeze bottle thing that we've got that we use. And Ron puts it on himself and he put some inside me and it helps us with are sexual activity. Um… I can't say it is as much fun as it used to be though because they're still great deal of vaginal dryness."
What can I do if I have pain or discomfort when I try to have intercourse?
- Let your partner know what is painful
- Try different positions
- Use additional lubrication (gels or creams such as K-Y jelly®, Astroglide® or Replens®; can also use glycerin or saliva; "DO NOT" use Vaseline®, Vicks Vaporub® or any other petroleum-based product)
- Increase time for sexual arousal before trying intercourse
- Take your pain medication prior to beginning sexual activities
- Do not have intercourse if you have vaginal sores or heavy bleeding from radiation therapy or if you have a low white count (check with your provider first)
- If you have vaginal narrowing you may need to use a vaginal dilator to keep the vagina open and flexible.
Dilator Set Sizes: Unit Front Diameter Back Diameter Length 1 - Dilator 3/4" [19mm] 7/8" [22mm] 3-1/2" [90mm] 2 - Dilator 15/16" [24mm] 1-1/16" [27mm] 4-5/16" [110mm] 3 - Dilator 1-1/8" [30mm] 1-1/4" [32mm] 5-1/2" [140mm] 4 - Dilator 1-3/8" [35mm] 1-1/2" [38mm] 6-3/8" [163mm] 5 - Handle Universal Handle fits dilators 1 through 4

- Your provider can tell you how to get a dilator.
- In place of a commercial dilator, you can use a small candle covered with plastic (saran-type) wrap or a condom (standard taper candle about 6-8 inches in length).
- Be sure to use a water-based lubricant such as K-Y jelly® or Astroglide® or you can use saliva to lubricate the dilator (plastic wrapped candle). Plastic wrap or condom is removed and thrown away after use.
- Over time, you will increase the size (width) of the dilator (or plastic-wrapped candle) to increase the size of the vagina.
- Having regular intercourse will also keep the vagina from narrowing.
- Some women may have a vaginal infection that can cause pain. If you have a creamy-white discharge or have itchiness in the vaginal area, you may have an infection. Contact your provider for the appropriate treatment.
What should I do if my interest in sex is less than I want it to be?
- For some women increased vaginal lubrication and decreased pain may increase your interest in sexual activities
- For others, drugs used to treat erectile dysfunction in men, such as Viagra® may be helpful
- Sexual counseling may help; ask your provider
- Talking with your partner and finding ways to be intimate and emotionally close also may increase your interest in sex
The Medicine Wheel: The Mind and Sexuality and Intimacy and Cancer
Jared, please insert the medicine wheel graphic here: NACES/MedicineWheel.png
How can the mind affect my sexual feelings and responses?
- Sexuality starts in the mind.
-
- Your brain is responsible for making you feel interested in sex.
- If you are anxious, sad or worried about your cancer and its treatment, you will probably be less interested in sex or sexual activities.
- Sometime you can create situations that do not exist or think things that are not true (such as believing that your partner will not love you if you do not have a breast or cannot have a child).
- Sometimes someone may make a comment that you take the wrong way or out of context. You may make a sexual decision based on what you think was said rather than what is meant.
What are some common worries/concerns about sexuality?
- Being embarrassed about physical changes such as hair loss (see hair loss branch) or scars (try wearing sexy lingerie or a partial clothing. Dim the lights. Use makeup that is made to cover scars.)
- Worrying that your partner will not find you attractive
- Worrying about how you will perform (or if you can perform)
- Worrying about how to explain your cancer and its treatment to a new sexual partner
- Being afraid your stoma will leak.
- Worrying that someone can "catch cancer from you" (they cannot)
- Feeling unattractive; disliking how your body looks
- Worrying that sexual activity can cause cancer (technically it cannot although the Human Papilloma Virus which is related to cervical cancer can be passed from one person to another during sex)
- Being afraid that having sex will make your cancer worse (it will not, in fact for some, intimacy and sexual activities actually make you feel better about yourself and more healthy)
Why is talking about sexuality changes so hard?
- Most of us do not usually talk about our sex lives with others, particularly strangers (even our healthcare providers)
- Some do not talk openly with their partners about their sexual needs and wants
- It often feels embarrassing to talk with others about sex
- It is often hard to find the right words to use
- Many use slang words or expressions that are not always clear to others ("I have a pain down there" may mean vaginal pain or it could be something else)
- Try writing down your questions/concerns to ask your provider so you will not forget or be as embarrassed (please see the sections on questions to ask your provider and common questions in other leaves on this branch).
- Talking to a specialist on sexuality may help; ask your provider to recommend an appropriate person.
- Even if you cannot have intercourse, a good "mind set" can promote intimacy and closeness, providing support and comfort.
The Medicine Wheel: Emotions, Sexuality and Intimacy and Cancer
Jared, please insert the medicine wheel graphic here: NACES/MedicineWheel.png
What emotional effects might I have because of changes in my sexuality?

label Lorecita Quintana, Santo Domingo Pueblo, diagnosed 1989 with colon cancer
"There was a lot of people, you know, that helped me along during that time. One of my, the person that comes to my mind is my partner. I think that if it wasn't for him, who knows what we went through, you know, and it was just very hard, very hard. Like I said if it wasn't for him to be there, you know, emotionally, and physically. I don't think I could have pulled this off by myself. There was another friend of ours, who is a very close friend of the family who also was there for me, and just helped me out a lot."
Jared: please insert PATIENTS_NACES_Survivors/  "I had this one friend that I had started dating after my husband had died. And when I had the breast cancer I told him, I said, you better find somebody else, you know, and he said no. He said, "I don't you know? I don't run out on people, when they need me", and so he took me to the radiation treatments along with I had friends to that did that."
"I had this one friend that I had started dating after my husband had died. And when I had the breast cancer I told him, I said, you better find somebody else, you know, and he said no. He said, "I don't you know? I don't run out on people, when they need me", and so he took me to the radiation treatments along with I had friends to that did that."
- Some may feel anxious, frightened or fearful because you do not know how long changes to your sexuality may last or you are worried you partner may not be interested in you anymore.
- These feelings may lead to decreased arousal or interest in sexual activities.
- Some may feel frustrated and angry because your life, including your sex life, has changed. You have to figure a "new normal."
- Some may be having cancer or treatment-related side effects that leave you fatigued or unable to sleep or think clearly.
- Some may be feeling strong or empowered because:
- You are using strategies to maintain your sexuality.
- You and/or your family are meeting with your traditional spiritual healer more often and getting into better spiritual balance.
- You are eating and exercising everyday to maintain/improve your health.
- Some may be upset about how your body has changed during your cancer treatment or how others are reacting to the changes in your body.
- Some may have mood swings (sudden depression, fatigue, anger)
- Some may feel that worrying about sexuality is silly or not important in the face of being cured of your cancer.
- Some may be envious of others who are healthy or who do not have to deal with cancer treatment and all the other difficulties you are facing.
- Some may be sad, depressed, angry or feel a deep sense of loss about no longer being able to have children
- You may feel less like a woman; less feminine or less a man; less masculine
Jared, please insert CeCe Whitewolf's photo here: PATIENTS_NACES/Survivors/Whitewolfe_CeCe-2.tif
Label: CeCe Whitewolf, Confederated Tribes of Umatilla
Diagnosed 1998 with breast cancer 
"We need to talk about, you know I'm going to say things that might be embarrassing to people, buts that's OK because I need you to listen to me. One of the things that has happened because of my chemo, is Ron and I… sexual activity has really changed from what it was before we went though this journey with cancer. We used to be a very sexually active couple, that's what attracted us to each other long time ago, 25 years ago, and we're still sexually active now, but it's not the same. It's not the same, not because I lost the breast, Ron told me one time, in fact I was giving a talk. I explained to him I said well, people were worried Ron that you would see me differently as a person who wasn't very sexual. And I said you've always been a boob man Ron, and he laughed and he said, "CeCe, I've only got one mouth, and you've only got one boob now so we have no more problems." So, you know, having one boob is no biggie as far as Ron's concerned and no biggie as far as I'm concerned, either."
How can my relationships be changed by cancer?
-
- Being ill with cancer or any other disease can change your relationships
- Worry, fear, anger, and increased stress are common when you are diagnosed with cancer
- Usually, if a relationship was good before you were diagnosed with cancer, it will stay god. If you were having problems before your diagnosis, they often get worse, or at least do not get better.
- Your role in your family may change. Others may need to do the things you usually do. This can be due to being in the hospital, being fatigued, or having nausea or pain. When family and friends offer to help, let them.
- Know that some may want to take care of you and not let you do anything. This can make you feel unneeded
- Ask people to do specific things for you like picking up your children after school or cleaning your bathrooms. Most will be glad to have something specific to do.
- Your future plans may need to change. This could be anything from having a child to taking a vacation to the job that you have.
- Oftentimes your relationships with your friends change. Some who were close will drift away. Others will remain close. Others who were not close friends may become close as you go through treatment. These people usually remain close friends after treatment as well.
label: Abe Conklin, Ponca-Osage, diagnosed 1987 with prostate cancer 
"My wife was very, how would you say . . . was very helpful, in her ways of being helpful to me. She stuck by me, she made me go to the doctors. She stuck by me when I went to the hospital, through surgery. So she was a very helpful, caring person and I appreciated it. She stuck by me, always through it."
Label: Bonnie Craig, Blackfeet, diagnosed 1991 ovarian cancer 
When something like cancer occurs in an Indian family, you deal with the extended family. You also deal with your core family. The core family, I think, is surrounded and protected by this larger extended family. My news of being diagnosed with cancer was the same as death occurring in our family system. My husband's younger than me. We're very close, and the day that I had to go home and walk in the door and tell him what the doctor said, you know, I wish that I didn't have to see that look on his face because it was absolute fear. Because he asked me, "You're going to live, aren't you." And nobody knows that.
What are some important things to know if I have a partner?
-
- Even though you are the person with cancer, it may be your partner who has problems with sex
- Sometimes your partner may be concerned about you and the changes happening to you and loose interest in sex
- Sometimes your partner may be afraid that cancer can be spread through sexual contact
- Your partner may be afraid to touch you for fear of causing pain or harm
- You partner also may not understand that your decrease in interest in sex is due to your cancer or cancer treatment and not your lack of interest in your partner
- Your partner's sexual drive may have changed or may even be increased. You should talk about the differences in your present interest in sex and find ways to satisfy each person's sexual needs within your relationship (such as cuddling or touching without intercourse)
- If you have fatigue, you may wish to look at different positions for intercourse or choose a time of day when you are less tired.
- You should plan to take your pain or nausea medicine before you begin sexual activities
Label: Patricia Horse Johnson, Kiowa, diagnosed 1985 with breast cancer 
"Martin is very, very supportive. He was just really in full support of me. Went into the hospital with me and never left until I came out. He carried me very well through that first experience with breast cancer. It was something that neither one of us had ever even dreamed would touch us but at the same time, he was there when I needed him. The rest of my family, they were just going along with whatever we wanted to do and we're a praying family, so they would gather around and have a round of prayers."
What can my partner do to help me?
- Your partner can help you by:
- Showing love and affection
- Talking with you about your interest and feelings about sexuality
- Taking cues from you and letting you go at your own pace
- Showing you affection in other ways than having intercourse such as cuddling, holding, hugging, and touching.
- Working with you to manage changes and find solutions
- Seeing a counselor together (as needed/desired)
What can I do to help myself?
- Remember that:
- You are loved for who you are, not just your appearance
- We are all sexual beings
- Survival often overshadows sexuality
- Sharing feelings is important
- Expect the unexpected
- Give yourself time; be patient
- Share what you want to share when you are ready
- Take the pressure off intercourse, try touching, just being together
- Do not let your diagnosis dictate what you can do sexually, do what feels right
- Plan sex around your changing energy levels
- Ask for help if/when you need it
- Stay as physically fit as possible
- Eat well
- Get plenty of sleep
- Be open to possibilities
- Do not be afraid to try something new
- Look for/try to maintain a sense of humor
- Trust in yourself and your partner
- Use plenty of water-soluble lubrication
- Do not forget to use birth control and protective measures that fit for your age and lifestyle
- Remember that sexual toys/devices may be good to add to your normal activities
What if I don't have a partner?
- Even if you do not have a partner, you can still have a personal sex life
- If you have a new relationship, you may wish to start slowly and then build your relationship
- If you want to have a new relationship, you will have to decide when to talk about your cancer and what you want to share. It may be best to wait until you are sure that the relationship is more than just a date. It is up to you (some tell on the first date; others wait until they are closer to having intercourse).
- You may wish to practice what you want to say before you say it
- If the relationship does not work out, do not assume it is because of your cancer. Not every relationship works out even without a cancer diagnosis.
- Use your family or friends for love and support through the cancer experience. You need to feel cared for even if you are not in a sexual relationship with someone.
Label: Dilly Adsuna, Alaska Native, diagnosed 2003 with breast cancer 
"So I went through my treatment alone, and that was the hardest, hardest thing to do. I think for someone to go through chemo treatment and radiation it would be very good if they had… have somebody there with them."
Label; Anonymous Native America Breast Cancer Survivor, Diagnosed 1995 with Breast Cancer 
"… this an experience that would help my friends understand and my family understand what I was going through because I couldn't verbalize it, I couldn't tell them how much this was hurting me. Even though it wasn't any direct pain, it was the pain inside that was hurting my spirit. So by doing those things, I was getting some help. By having them just touch me, you know, just that that connection. Those are the things that I, I hold precious in my heart"
What if I am two-spirited (gay, lesbian, transexual, transgender)?
-
- Having a satisfying sex life is important to all people regardless of whether they have an opposite sex or same sex partner
- The loss of some sexual function may be difficult, causing sadness, anger and frustration
- The same concerns that affect an opposite sex partnered relationship or being single will affect the two-spirited person
How do I manage my body image changes?
Label: Christine Mangiati, Italian (Non-Native), Dx 2003 Breat Cancer 
- Partially covering your body with clothing or sexy underwear may be easier than being naked
- Use dim or indirect lighting to mask body changes
- It may be helpful to face away from your partner
- Sex may be easier if you are lying on your side (takes the pressure off any scar or a stoma)
- It may be helpful to look at the changes in your body in little pieces rather than all at once (try removing one piece of clothing at a time, looking and getting comfortable with that part before looking at more of your body; look at your body through a filmy nightgown)
- You may need to find other ways or areas to be touched and caressed through self-stimulation (touching and looking at your body is really okay)
How do I resume sexual activities?
-
- Be open to change in who starts sexual activities or what positions you use.
- Take your time to learn/relearn what feels good/gives you pleasure.
- Start slowly with kissing, cuddling, or touching; over time move to intercourse
- Talk with your partner about your concerns and what feels good (or does not); listen to your partner's concerns/thoughts
- Plan sex around when you are less tired; take medications for pain, nausea or other medical problems before becoming intimate
- Using/sharing sexual fantasies may be helpful
- Be patient with yourself and your partner; keep trying
- Maintain a sense of humor
- Remember problems have solutions
- Make sure you have privacy but do not be afraid to try other places than usual for sexual activities
- Do not let embarrassment keep you from trying new things or talking about sex
- Make sure to use birth control methods that fit for you and your partner (not everyone who has cancer treatment is infertile)
- Pregnancy during and immediately after cancer treatment should be avoided
Label: CeCe Whitewolf, Confederated Tribes of Umatilla
Diagnosed 1998 with breast cancer 
"One of the things that the doctors told me about, and again nobody told, tells me this thing I was growing up. I didn't know, one of the reasons I was getting bladder infections, because I'd get bladder infection after Ron and I would have sexual intercourse. And the reason I was getting bladder infections was because I wasn't going to the bathroom, within half an hour of after our sexual intercourse, and I thought that's an interesting and one. A physical P.A. fellow at Kaiser told me go to the bathroom after sexual intercourse. I said Oh, okay so ever since, I've been going to the bathroom after sexual intercourse. I don't get bladder infections."
Are there times when I should not have intercourse?
-
- You should wait at least 6 weeks after pelvic surgery to have intercourse; ask your provider for a specific length of time
- Either do not have intercourse or be sure to use appropriate birth control method(s) during active cancer treatment (and at for at least one month after completion of therapy)
- You should avoid sex if your white count or platelet count is low (if you have neutropenia [new-tro-peen-ee-ah] or thrombocytopenia [throm-bow-sigh-toe-peen-ee-ah] or you have bleeding)
Are there counselors or sex therapists available to help?
- There are people trained to help you with sexuality problems
- If you think things are not getting back to normal, you may want to seek professional help
- Your healthcare provider can give you a recommendation or make an appointment for you.
The Medicine Wheel: Spirituality, Sexuality and Intimacy and Cancer
Jared, please insert the medicine wheel graphic here: NACES/MedicineWheel.png
Label: Rosanne Wyman, Upper Mohawk, Six Nations Indian Reserve, diagnosed 1987 with cervix cancer 
"When I was about 5 months pregnant with my youngest son who's 21 right now, I had my pap smears was suspicious. They said I had, like, precursors to cancer. We went through all the medical stuff that okay the doctor told me that I was going to have a biopsy. I got right to the point where I was on the table, and then all of a sudden he tells me, well, I'm gonna do this, this, this. This little detail that he forgot to tell me, that you might lose your baby. Well, this was no little detail to me, it had an impact on my life. I figured, two children were plenty for me and this was going to be my last one, and hoping it was a girl. But a boy and he's been the light of my life too. But, anyway, the doctor says, you might lose the baby. He says, well the baby is abnormally small anyway, if you lose it, that's ok, you can have another one! I thought, what a cold person! Is this because, was I treated like this because am I Native? Is it because I'm Native? That, you know,like he didn't fully explain all the details? And just figured well bang, she's just going to go through with it, do what she wants, do what I want and that will be the end of it. But, I objected, no way, I'm not going to do that. I don't want to lose my baby, and I didn't. He got mad and refused to be my doctor. So, that was it. You know, I had to find another doctor, to get a, to have the baby delivered. And this abnormally small baby he's three hundred pounds today. He weight lifts, he's about 6' tall, and as healthy as they come. I'm glad, you know, I put my life on the line for him. He's certainly made every moment worth while. This was all from like basically, everything stems from my spirituality, my strong faith. The belief that the Creator was going guide me in the right direction. And He has."
General Concepts
- Every Native culture includes sexuality and intimacy as part of a healthy family life.
- Some religious teachings say that any touching of one's body is evil and wrong.
- Common sexual practices may often include touching private areas of one another's bodies.
- Touching your own body is important for breast health. You need to know what your breasts feel like to know what is normal for you (see monthly breast self examinations in "Get on the Path to Breast Health" module 6 )
- Touching your body does not cause cancer.
- Most tribes have some traditional rules about talking about sexuality or intimate activities. Generally, it is discouraged.
- This is to display modesty and show respect for the Creator's spiritual gift of sexuality.
- Humor may be used, but not at another person's expense.
- Crude talk and joking should not be used as it may violate spiritual sacredness
- Mothers or Aunties are traditionally the sexual educators for their daughters / nieces.
- Fathers or uncles are traditionally the sexual educators for their sons / nephews.
- Healers are usually required to be of the same sex as the person if the problem is sexual. For example, a woman who is having a lot of bleeding after a mastectomy goes to an elder women healer for help as well as to the western medical provider.
Sexuality and intimacy usually are intertwined with spirituality.
- Each Native culture includes specific beliefs of how the spirit, sexuality, and intimacy are intertwined.
- Most include that the male and female roles within the family are related spiritually and those spirits become stronger with sharing intimately with one another. that the spirit of union and family is part of sexuality and that our spirits join
- In the past, most if not all tribal traditional practices included several types of sexual or gender ceremonies, for example, puberty ceremonies. These are still conducted today by many tribes. Puberty ceremonies differ greatly for males and females. All are designed to instill respect for one's body and sexual functions. Many of the female puberty ceremonies emphasize the blessing the Creator grants to the body as a "life giver".
label: "Punkin" Shananaguet, Pottawatomi/Ojibwa, Cancer Advocate 
"We believe in that sacred sense of touch, healing. We believe that touch is healing in itself. Traditional knowledge that has been debased and devalued by the influence of the church and boarding school area, the association of self exam for masturbation, therefore perceived as sinful to touch yourself. Therefore, our grandmothers lost their connection to their own body and personal health practice management."
-
- Even if a woman learns later in life that she cannot have children, once puberty ceremonies are completed, the woman's role in the community is of a protector of both the young and the elders.
- Tribal female elders state that these ceremonies help young girls behave in more responsible ways in comparison to others who do not take part in these ceremonies.
- Gender ceremonies include distinctive traditional naming ceremonies for males or females. Some tribes later in life also do two-spirited ceremonies to acknowledge and respect lesbian, gay, bisexual people. Those who are transsexual are treated differently by individual tribes.
- Pregnancy ceremonies for a blessed and healthy child are also conducted with the entire family by individual tribes. There are ceremonies that include the placenta for spiritual practices or to protect the health of the infant and throughout life.
- Ceremonies exist for the couple who have a miscarriage
- Ceremonies also exist for people born with or who have physical, mental, emotional or spiritual problems.
- Spiritual ceremonies are used by many for couples living together (same sex or mixed sexual relationships).
- Wedding ceremonies include requests for the Creator to bless the union of the couple and for their families.
- Some traditional tribal practices do/did not recognize divorce. However, divorce ceremonies are becoming more common. They may be contemporary or traditional. These ceremonies allow the former partners' spirits to separate without damage. Getting or being divorced does not cause cancer.
- Any damage or removal of sexual organs usually requires some type of spiritual ceremony. This may be one or a series of related ceremonies conducted over 6 months period of time.
- This may allow a woman to be intimate with or without sexual intercourse.
- A woman who has a hysterectomy may also take part in a healing ceremony of her spirit.
- Some traditional tribal beliefs specify that women cannot take part in sexual intercourse until they go through such a ceremony. This protects both the woman and their sexual partner.
- A respected elder female healer from the woman's own tribe or a related tribe usually performs the ceremony.
-
Sexual behavior and spirituality are "NOT" always intertwined
- Rape, molestation and incest are examples of violence, force and unhealthy forms of showing power over another. They are not about sexuality. Many tribes believe that the person who rapes or molests is possessed by evil spirits or is cursed by another.
- These behaviors were not part of any Native historical traditional behaviors. They are not acceptable behaviors today.
- Cancer patients who were victims of such behavior usually require a combination of ceremonies for both the violence and the cancer.
- Rape, incest, molestation "fracture" the spirit of the victim.
- When cancer occurs, even if the fracture was healed through traditional ceremony, the cancer spirit may open the wound.
- Another ceremony may be needed for healing.
- Cancer is not caused by violent sexual behavior
- Sleeping with someone else's spiritually sanctioned partner may also have a similar wound effect. While this behavior may increase one's risk for cervix cancer, in and of itself, sleeping with someone else's partner does not cause cancer.