Side Effects - Lymphedema
Welcome to the lymphedema branch of the NACES Quality of Life, side effects
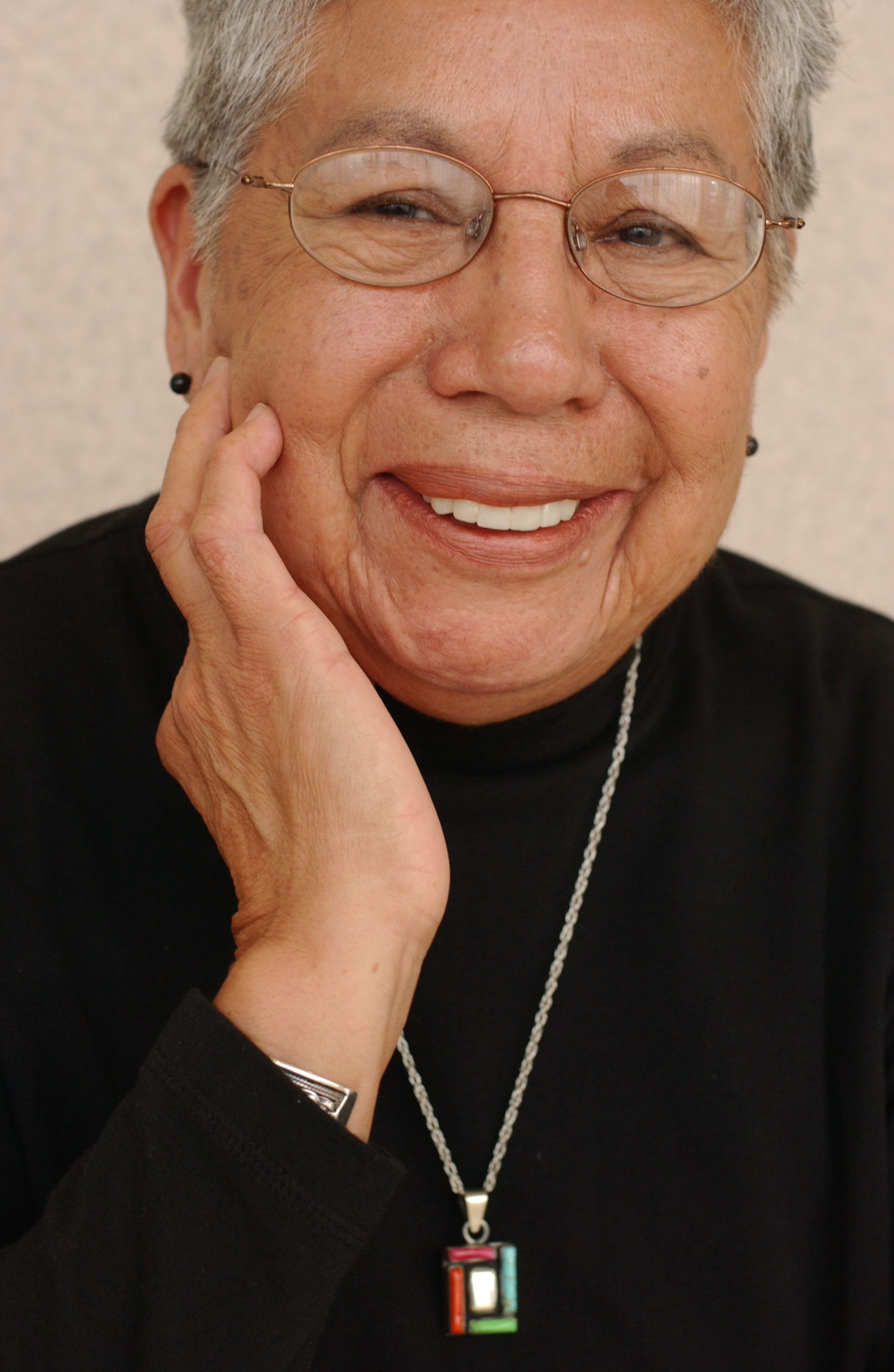
The authors of the lymphedema pages are Linda Burhansstipanov, MSPH, DrPH, Cherokee Nation and Jeffrey Koser, C.S.C.S.
The purpose is to help you understand lymphedema and how you may be able to prevent, control or reduce its effects
- Lymphedema is swelling of the arm(s) or leg(s)
- It is caused by damage or removal of the lymph nodes
- It can happen to any patient
- A lot of patients do not recall receiving information about lymphedema
- It may be painful
- It also may be hard to deal with
Who gets lymphedema?
- Some patients never get lymphedema
- Others do
- Some get it once, then never again
- Some get it over and over again
- Medical scientists do not know why ... yet
- But if you had lymph nodes removed or damaged, you have a lifetime risk for lymphedema (it can happen to you next week, 20 years from now, or never)
- If you have symptoms, and you've never learned how to manage the symptoms, you need to see your provider right away (within the same day of noticing the symptoms, if possible)
- The longer the delay, the more likely you are to have serious problems
NOTE: This section includes information about lymphedema (swelling) of both the arm(s) and leg(s)
- Breast cancer patients usually only get the swelling in the arm(s) where the lymph nodes were removed
- If patients had lymph nodes removed near their groin, they can get lymphedema in their legs
QUESTION: Do you think cancer-treatment related lymphedema is more common in men or women?
1. Men
2. Woman
3. Don't know
Answer
"Women are twice as likely as men to have lymphedema after having lymph nodes removed as part of the cancer diagnosis and surgery."

Robert Judkins, Cherokee, diagnosed 1993 with testicular cancer
Doctor says, "Well in 90 days you have to have another surgery to take out your lymph nodes, sexual lymph nodes".
Robert, "So I still don't have insurance and I know that, that it's going to be a big ordeal. So I do the wrong thing. I go a year and just forget about it."
Lymph nodes are removed as part of a cancer diagnosis. They also can be damaged by radiation.
What is lymphedema? Lymphedema is:
- Extra fluid in your arm(s) or leg(s) where you had any lymph nodes removed or damaged
- A side effect from having lymph nodes removed during surgery
- A side effect from the doctor taking out some of your lymph nodes
- A chronic condition
- Not curable
- Manageable for most people
How soon does it happen? Lymphedema may occur:
- Not at all to you
- Immediately after your cancer treatment
- 1 to 2 years after your cancer treatment
- Many years after your cancer treatment
- After your treatment, but started
- Because of an insect bite or some other minor injury
- After a lot of physical activity
- After a plane trip
NOTE: Once lymph nodes are removed, you may get lymphedema at any time for the rest of your life
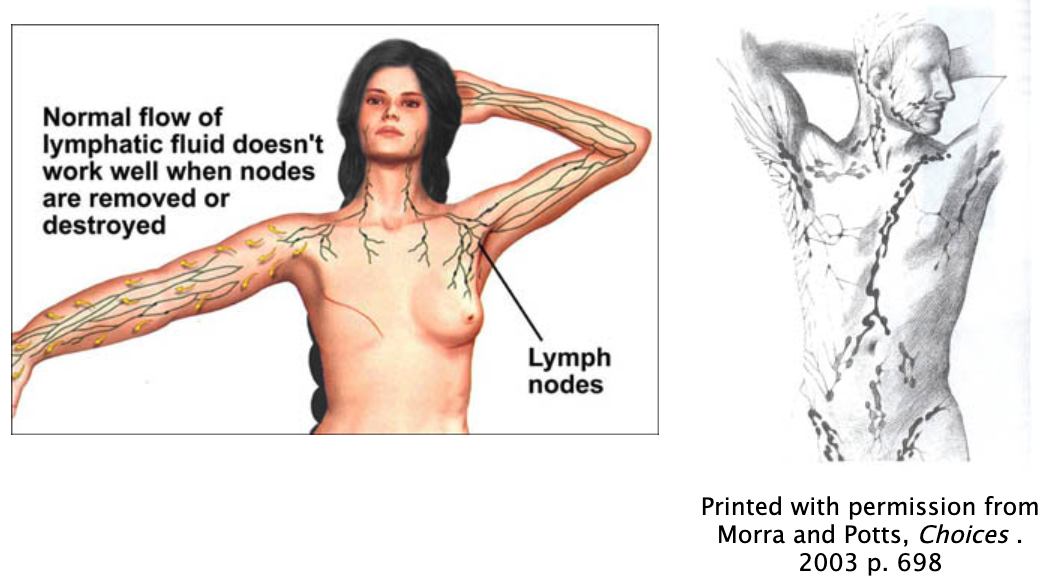
What are lymph nodes? Lymph nodes:
- Are small glands
- Help drain fluids from your arms and legs
- Help keep good fluid balance in your arms and legs
- Get rid of
- Infections (like harmful bacteria)
- Waste materials (waste happens even when cells act normally)
- Poisons in your body (like from medications)
So many new words are used that most people don't understand a lot of what is happening to them. The lymph nodes help fluids to drain from your arm. They are important in fighting infections
"But the thing that I wasn't ready for was the 17 lymph nodes that they had to remove along with my breast. And I said OK, what does a lymph node do anyway? What do I need it for?"
What is the lymph system?
- It is small tubes (like blood vessels) that are in your body tissues. These tubes lie alongside your blood vessels.
- It contains infection-fighting white blood cells called lymphocytes.
- Lymph nodes are small glands that help balance fluids and get rid of waste materials.
- The lymph system also includes the spleen, thymus and bone marrow (Marion and Potts, Choices 2003, pp. 697, 196, 197, 422, 423)
Where are lymph nodes in my body?
QUESTION: How many lymph nodes do most people have in their entire body?
- About 50
- Between 51 and 100
- Between 101 and 300
- Between 301 and 500
- Between 501 and 700
- Don't know / Not sure
ANSWER:
The body has between 501 and 700 lymph nodes
(the number of nodes varies from individual to individual).
About half of the nodes are in the middle of your body (stomach or abdominal cavity).
The lymph nodes near your armpits and groin have about 100 nodes.
Thank you, Saskia R.J. Thiadens R.N., Executive Director, National Lymphedema Network
Why do I need lymph nodes or the lymph system?
- To help prevent infections and injury
- To help fluids drain from your arms and legs
Why is lymphedema a problem? The lymph fluid:
- Is not able to drain from your arms
- May contain bacteria or wastes that stay in your arm(s) or leg(s) (soft tissues).
- When bacteria and wastes stay in your tissues (rather than draining away), they have time to grow and become infections.
- Causes pressure that may also cause pain
Why did the surgeon take some of my lymph nodes out?
- The providers need to look at your lymph nodes to see if they have any cancer cells in them
- If they see cancer cells in one or more lymph nodes:
- Then your cancer may have spread to other parts of your body
- The type of treatment you get will be different from someone else who does not have cancer cells in their lymph nodes
How did the provider damage some of my lymph nodes?
- The lymph nodes are very small. It is easy for the surgeon to accidentally cut a lymph node or damage one during surgery
- Radiation can also damage the lymph nodes
When are lymph nodes removed?
- Lymph nodes may be removed at the time of the first biopsy. Other times lymph nodes are looked at or removed after receiving the biopsy results.
Ruth Demitt, Athabascan/Tanacross, diagnosed 1985 with breast cancer

"In August they did a biopsy and we find out it was breast cancer. It was located by the nipple... Then a couple of weeks later they did a biopsy on the lymph nodes and had to take three out and one of them was positive."
- Sometimes things happen so fast you may not even realize what is happening.
"Then I went back five days later and they removed the fifteen lymph nodes and glands, and that was the way it happened, and it all happened so fast, it was kind of a surprise."
Who is likely to get lymphedema?
- Some patients are less likely to get for lymphedema; especially if other lymph nodes are not damaged during surgery.
Arlene Wahwasuck, Prairie Band Potawatomie Tribe, Diagnosed with breast cancer in 2002
"My lymph nodes were negative and the size of the lump was small"
- It is not really clear why some patients have no problems with lymphedema but other patients have many problems.
- Breast cancer patients who had surgery may get lymphedema
- This includes a simple mastectomy, lumpectomy or any other type of surgery that includes the lymph nodes
- Lymphedema also happens from radiation that damages the lymph nodes
Do only breast cancer patients get lymphedema?
- No, other cancer patients who have lymph nodes removed may also get lymphedema:
- Prostate cancer
- Uterine cancer
- Cervical cancer
- Testicular cancer
- Colorectal cancer
- Pancreatic cancer
- Liver cancer
- For some of these other types of cancer, the legs are more likely to swell than are the arms
- Some people who are not cancer patients also get lymphedema
- Their treatments may be the same as for cancer patients
What are some other facts about cancer-related lymphedema?
- It is about twice as common in women than in men
- Only about one out of every five people who have lymph nodes removed as part of their cancer diagnosis gets lymphedema
- It may happen right after your surgery or it may not happen for years after you have recovered from your cancer experience
- Even though a lot of people get lymphedema, many patients do not remember the provider ever telling them about it
- It does NOT mean that your cancer has spread
- It is important to do daily activities to help prevent it
What is "primary" lymphedema? (Not related to cancer diagnosis or treatment)
- These types of lymphedema are different from the type of lymphedema that cancer patients get (March /April 2006; nursing made incredibly easy! p. 27)
- "Congenital" means that a baby is born with damaged lymph tissue or is missing tissue that makes up the lymphatic system. This has nothing to do with cancer
- "Lymphedema Praecox" is also a condition the person is born with. It shows up anytime between birth and 35 years It also has nothing to do with cancer
- "Lymphedema tarda" is also a condition a person is born with but doesn't show up until after age 35
How is cancer-related lymphedema labeled?
- Damage to the lymph nodes from surgery or radiation is also called, "secondary" lymphedema
- "Mild acute lymphedema" lasts for only a few days
- It is not usually painful
- "Acute lymphedema" occurs 6 to 8 weeks after surgery or radiation
- The arm or leg feels warm or hot, and is painful
- "Superficial" is caused by an insect bite or injury to the arm or leg
- The inflammation is likely to begin within 24 hours of the bite or injury
- The arm or leg feels warm or hot, and is painful.
- "Delayed Acute lymphedema" may occur long after the surgery or radiation
- While it usually begins 18 to 24 months after surgery, it may occur many years after treatment is completed
Medicine Wheel: The Body and Lymphedema's Impact

What are the symptoms of lymphedema?
- Swollen arm(s) or leg(s) that may become up to twice the size as normal or have large folds of tissues, bumps or creases
- A feeling of heaviness or fullness in the arm or leg
- A tight feeling in a hand or foot
- Changes in skin (rough, dry, hardening)
- Difficulty moving the arm(s) or leg(s) (less flexible than normal)
- Infections or sores that do not heal
- Skin that "pits" or remains indented for 5 seconds or longer when you gently push your finger on the swollen arm, hand, leg or foot
What are ways to help protect my body from getting lymphedema?
- You must avoid pressure, infection or any injury to your swollen arm(s) or leg(s)
- If you use "constriction" garments or bandages they need to be fitted to you by a trained provider. They only last for about 6 months and you usually will need more than two sets.
- Even when the arm(s) or leg(s) that had lymph nodes removed are NOT swollen, you should:
- Not have blood pressure taken in that arm or leg
- Your provider can take blood pressure from another body part
- Remind the provider that you have had lymphedema so that s/he understands your concern
- Not get any shots or injections in the arm(s) or leg(s) that had lymph nodes removed or damaged
- Not have blood taken from the arm(s) or leg(s)
- There is some debate about how safe it is for someone who has never had lymphedema to have blood drawn from the arm(s) or leg(s) that had lymph nodes removed
- Ask your provider
- Not wear tight-fitting jewelry, including rings, wristwatches, bracelets or cuff links
- Not wear elastic cuffs or tight sleeves or pants (like sweat pants with elastic cuffs that are tight enough to leave indentations in your ankles)
- Not carry anything heavier than 3 pounds (fish, game, groceries, purse, backpacks, suitcases)
- Obviously this is a general recommendation
- If you are very strong, you may not have trouble carrying more weight. But if you have any problems talk with your provider about how much weight is "safe" for you to carry
- Not carry a purse or backpack of any weight that straps and hangs around your arms. Same caution note as in the previous item
- Not carry heavy lances, staffs or other traditional items with the arm that has had any lymphedema in the past or present
- Be careful of how you move or use your arm(s) or leg(s)
- The physical therapist can tell you what you can and cannot do
NOTE: These are general guidelines
- You need to work with your providers to find out how each of these guidelines relates to you, or can be modified for you and your daily activities
- For example, if you have never had a problem with lymphedema or if you are very strong, you may be able to lift more than 3 pounds with the arm that had lymph nodes removed
- Please ask your provider
 AI/AN cancer survivor who requested to remain anonymous: "While attending a wellness gathering for Native Survivors, the participants did a fly fishing exercise that moved their arms so that one of their elbows was above their shoulders and then moved their arms forward like they were casting the fishing line. The exercise caused an elder's lymphedema to immediately swell. She had to go home and it took three weeks to get the swelling down in her arm. "Fall 2004
AI/AN cancer survivor who requested to remain anonymous: "While attending a wellness gathering for Native Survivors, the participants did a fly fishing exercise that moved their arms so that one of their elbows was above their shoulders and then moved their arms forward like they were casting the fishing line. The exercise caused an elder's lymphedema to immediately swell. She had to go home and it took three weeks to get the swelling down in her arm. "Fall 2004
- When you take a plane to fly somewhere, you may want to wear your compression sleeve or bandages
- The air pressure in some planes changes enough to make some people more likely to get lymphedema
- Get up and walk around for about 10 minutes every hour (obviously do this more frequently if you feel it is helpful to you)
- Personal daily cleanliness and behaviors may need to vary
- If you shave your underarms (a lot of us don't have much underarm hair):
- Use an electric shaver rather than a shaver with a razor blade
- Ask your provider when it is safe for you to shave
- Do not shave until your lymph node surgery wounds are completely healed
- Clean and change the shaver heads of the electric razor often
- If you have breast prosthesis, get a type that does not weigh much
- You may need to wear soft pads under your bra straps
- Do not wear bras with under-wire support
- Do not wear bras with thin straps
- Wear loose fitting but secure rubber gloves when washing dishes, cleaning fish or game and washing gardening or other tools
- Wear long oven mitts to protect your hands and forearms from burns when cooking (both indoors with the oven and stove, and outdoors over the open fire or smoking fire)
- Wear warm sweaters, coats, gloves and boots when in cold weather
- Keep the arm(s) or leg(s) covered when outside to avoid accidental cuts or punctures
- Use sun screen to avoid sunburn (you are more likely to burn after your cancer treatments):
- Even if you never used to get sunburned)
- Use insect spray to help prevent insects from biting or stinging your arm(s) or leg(s)
- Use a thimble when sewing to avoid punctures
- When flying or riding in a car for more than an hour:
- Wear a compression sleeve or wrap your arm
- Drink lots of water
- Avoid salty foods (like cheese, chips, sodas)
- Get up and out of your seat to walk around for at least 10 minutes every hour
- Wear a lymphedema alert bracelet or necklace in case you have a problem or accident and are not conscious
- Have your provider give you an antibiotic prescription in case an infection begins when you are far from the clinic
- Talk with your provider about how to decide if you should begin to take this medication, how much to take and for how long
- Schedule an appointment with your provider to discuss this infection to make certain it is cured or if it was something other than an infection
- For lower body (leg(s) and feet) lymphedema, avoid crossing your legs, sitting or standing for long periods of time and wear well-fitted shoes (you may need to have two different sizes of the same shoe to not make the swollen foot too tight)
What are other prevention behaviors I can do to avoid lymphedema?
NOTE: (http://www.lymphnet.org and Cure: Spring 2003, pp. 58-61; http://www.curetoday.com)
- Get to your healthy weight (Avoid obesity or extreme thinness)
- Keep skin clean and well moisturized
- Do a daily "skin check"
- See if you have any cuts, burns, bits or other injuries
- Treat the injuries as directed by your provider.
- This usually includes using an antibiotic cream
- See if you have any redness, red streaks, tenderness of swelling
- Keep your arm and underarm clean and dry
- Pat your arm dry rather than rubbing it with a towel
- Look for hangnails or cracked or torn cuticles
- Keep your cuticles moist with cream
- Push them back
- Do not cut the cuticles
- Wear comfortable, loose-fitting clothing and jewelry
- Protect your arm(s) or leg(s) from injury
- Keep the swollen arm or leg raised on a pillow or something soft so that it is higher than your heart
- While sitting, sleeping, or traveling if possible
- Wear a compression garment (support sleeves or compression stockings)
How to manage lymphedema
- Lymphedema is managed based on guidance from your provider that is specific to you.
Why does it matter how quickly I get help for my lymphedema?
- Lymphedema can cause the arm or leg to be permanently swollen
- Early treatment may prevent the problem from becoming permanent
- If you notice even 1/2" swelling, redness, harness, or warmth in your arm, underarm or affected breast area, call your provider.
- Starting therapy before the arm or leg swells very much can help shorten the episode
Medicine Wheel: The Mind and Lymphedema's Impact on the mind and our mental functions

How does lymphedema affect the mind?
- The pain and discomfort can cause problems with your ability to concentrate or focus on a topic.
- You may find yourself needing to learn a lot more about lymphedema
- One of the best resources is a web-site called the "National Lymphedema Network" http://www.lymphnet.org
- Learning more about the problem helps you learn what you can do to reduce the likelihood of having recurrent or continued lymphedema and how to manage it
- Trained healthcare providers can teach you how to do your own "manual lymph drainage" correctly so that you can begin to get control of the lymphedema even before you are able to get back in to see the provider
- You may learn about different organizations that will help fit you for a compression garment or bandages at low cost or no cost
- You can learn how to exercise is a safe way from trained healthcare providers and therapists
- You can find financial resources to help pay for the lymphedema care. Several are listed on the financial resources branch. Others are specific to federal programs like the Women's Health Care Act of 1998 that specifically mentions lymphedema care to be covered by most health insurances. Medicare has limits on which parts of lymphedema care it can pay for and which it cannot
Medicine Wheel: Emotions and Lymphedema

What are emotional effects of lymphedema?
You may feel frightened because:
- It is the first time you've had to deal with it and you don't know what to expect, what you can do to manage it, or how to help prevent it from becoming a serious problem
- You've had lymphedema before or heard stories about it
- You think the lymphedema means your cancer has spread, but the swelling is rarely related to any new cancer
You may feel frustrated and angry because:
- You've been doing really well and taking good care of yourself
- Sometimes medical scientists have no idea why lymphedema gets started
- You've had such a hard time lately and this is "just one more thing"
- It is frustrating, but there are things you can do to help keep it under control.
- You feel like you have no control over what is happening to you
- But this is not true
- You never felt like you were constantly being reminded you had cancer, but now you have to deal with this side effect of your disease
- But lymphedema is hard to ignore and you should not try to ignore it
- You've been able to hug your family and friends again, and now you and they both have to be careful of hurting you again
- You are "fragile" in others opinions or in your own opinion
- You are unable to sleep or rest comfortably and are irritable from lack of sleep
- You cannot go into Jacuzzi's or steam rooms with your friends or families when staying at hotels. You feel excluded or punished
- Some co-workers or members of the community may make mean comments to you, just to be hurtful
You may feel strong and empowered because:
- You are taking active steps to keep the lymphedema under control
- You and/or your family are meeting with your traditional spiritual healer more often and getting into better spiritual balance
- You are eating and exercising everyday for overall good health, and these behaviors help reduce the likelihood of another episode with lymphedema
- The lymphedema has helped you get your weight to what medical doctors call "normal weight"
You are likely to feel self-conscious because of the odd shape of your arm(s) or leg(s)
- You may have to keep the arm(s) or leg(s) covered up when the weather is hot
- You have to wear clothing when going into the water when it is hot
- You have to have bottled water to drink while doing ceremony (different behavior from everyone else doing ceremony)
- You may have to sit near an exit door during ceremony to avoid getting too hot
- You are likely to want no one to touch you because of the pain
- You may have mood swings (sudden depression, fatigue, anger)
Medicine Wheel: The Spirit and Lymphedema

What are spiritual effects of lymphedema?
- Many Natives feel that they are spiritually out of balance because of the lymphedema
- Prayer helps many Natives heal and cope with the discomfort of the lymphedema
- Ceremonies need to be modified to avoid risk of infection
- Tell your traditional healer about the lymphedema and the limitations you must follow:
- No piercing or "rendering" of flesh from the swollen arm or leg
- No bindings of any type to the arms or legs
- No carrying of items heavier than 3 pounds (like a staff with beadwork and art objects)
- No kneeling on the ground if the legs are swollen
- No digging the holes in ground, or lifting poles for the lodge
- No vigorous dancing (like stomp dance ceremony all night long)
- No fasting (you need both food and water to help the lymphedema heal)
- No long walks to isolated places for meditation or vision quests
- No peyote or other Native American Church religious beverages while lymphedema symptoms are present
- No ointments or poultices packed onto the swollen arm or leg
- Allow other members of your family or your friends to do the ceremony in your honor
- You can pray with them but must keep the swollen arm or leg clean and free from cuts, lotions and avoid heavy lifting
- You can meditate at home or at the healer's home. But stay close to a phone and transportation if you need to get quick help while praying or doing ceremony
Exercise and Lymphedema
What is the goal of the exercise program?
- The primary focus of the exercise prescription provided will be to improve the overall quality of life of the individual throughout various modalities.
- Exercise guidelines
- Start your physical activity / exercise program under the supervision of a healthcare provider or therapist who is experienced working with lymphedema patients
- This person will help you personalize the activities to reduce the likelihood of you injuring yourself or making the lymphedema worse
- Do physical activity (such as gardening, cleaning the house, walking, swimming, or other exercises) only while your arm is wrapped or while wearing a compression sleeve.
GENERAL Instructions:
- Start your physical activity / exercise program under the supervision of a healthcare provider or therapist who is experienced working with lymphedema patients
- This person will help you personalize the activities to reduce the likelihood of you injuring yourself or making the lymphedema worse
- Do physical activity (such as gardening, cleaning the house, walking, swimming, or other exercises) only while your arm is wrapped or while wearing a compression sleeve
Caroline Shubert, Fisk River Inupiaq, diagnosed 1988 with breast cancer

"The three of us would go for walks in the neighborhood. I would deliberately swing my arms to try to get back the mobility and movement in my arms. I had exercises: walking your fingertips up the wall, I had to do that... Once I get them up there push down you know. Um, I spent a lot of time doing exercises, um and going for walks, I like the out of doors. After I was cleared to fly, I went up to the village. And mother was there. And the fish were running and it was so difficult because I had been cut from one side of the body to the other, the incision was healing, but I, I had very little strength in my arms. Hans and my brother, Johnny, would lift the fish up on to the table. Sometimes I could only cut two or three salmon and then I would have to go back and lie down. There is a lot of insulation across the area, and I found that even in the warmest weather I would get very, very cold."
- Wear loose clothing with wide waist bands and wrists and ankle cuffs
- Sit or stand tall and straight with good posture while doing your activities
- Take turns doing activities that use the muscles and then relax that group of muscles
- Keep muscles not involved in the activity relaxed
- In general, use slow, controlled movements while doing your activities
- A cadence of 3 seconds on the eccentric (easy portion) and 1 second on the concentric (hard or lifting portion) should be used.
- Isometrics or static hold exercises (planks) should be targeted for core specific workouts instead of exercises where the spine may be compromised (sit-ups, crunches).
- Do your activities once or twice a day, 8-12 repetitions whether unilateral or bilateral or follow your therapist's or provider's directions.
- Program should be progressed along bell shaped curve where intensity is gradually increased.
- Begin program with non-weighted exercises including both static (hold) stretching and dynamic (with movement).
- A rating of perceived exertion (rpe) should be used by client and kept at a low level to begin program and progressed gradually as long as there is no discomfort through swelling or pain. The scale starts at 1 (no effort) and moves up to 10 (highest effort).
- Resistance exercises (weighted) can be included after 1 month of non-weighted exercise giving the body adequate time to adjust to soreness and correct form and technique.
- Only begin resistance training if rpe remains low and no discomfort takes place.
- Aerobic exercises should be included at a low intensity (swimming, biking, walking) 4-5 days for 20 minutes a week to improve cardiovascular endurance and help to increase active blood flow.
Don't do:
- Anything that causes pain or cramping, unless your therapist needs you to do something uncomfortable for a while
- Fast, rapid, forceful movements
What type of physical exercises should I do to help prevent or manage my lymphedema?
- Your body works better when you have daily physical activity
- This is still true when you have lymphedema
- But, you need to do your activities in ways that will not hurt your arm(s) or leg(s) that had lymph nodes removed or damaged
- The therapist or rehabilitation specialist can help you find activities that fit your daily physical needs or exercises to help make your arm(s) and leg(s) less likely to have problems with lymphedema
- Exercise helps the muscles contract and this helps get the lymphatic fluid moving
- Deep breathing and drinking water also helps to get the lymphatic liquids moving
- Your daily life may include activities that are just as beneficial as any of the exercises described below
- Picking up a baby
- Cleaning fish or game
- Lifting a ream / package of paper for the office machines
- Raking dry pine leaves to help as a fire starter in the fire place
- Walking up and down stairs at home or at work
- Walking up and down hills outside
- Putting groceries away
- Shoveling snow or mud
- Dancing or teaching others traditional dances
- Here are some general guidelines (talk with your provider about how they can be changed to fit your physical condition):
Dynamic warm up exercises “upper body” (Most of these exercises can be done standing or sitting)
- NOTE: Show your provider the exercises below to get approval before you do "any" exercises
- Start and end the activities with good slow deep breathing
- Controlled breathing during stretching will allow for muscles to relax during exhale portion promoting a greater range of motion or stretch
- Breathing during body weight or resistance exercises should follow the pattern of inhaling on the easy portion (negative) and exhaling on the hard portion (positive)
- If you have trouble standing, you can do many of the exercises while sitting down
- But if you feel strong enough, try to do them standing as this will help build core strength
- If you have trouble standing, you can do many of the exercises while sitting down
- Start each workout with dynamic stretching and end with static (hold) stretching.
- The length of time you stretch for warm-up stretches will be repetition based
- Post workout static stretching should be 20 seconds per stretch or side if unilateral
- Neck rotation
- Face the east
- Turn your head to the right (south) then to the left (north)
- Do these 8 to 12 times, depending on how tight or comfortable the movement feels for you
- Tip your head slowly so that your right ear stretches to touch your right shoulder
- Keep your shoulders lowered and relaxed
- Slowly tip your head to stretch your left ear to try to touch your left shoulder
- Keep your shoulders lowered and relaxed
- Chin tucks
- Keep your chin level
- Gently and slowly pull your head and neck back on your shoulders (with the chin level)
- Gently and slowly push your head and neck forward (still keeping the chin level)
- Repeat between 5 to 10 times
- Keep your chin level
- Shoulder blade squeezes
- Squeeze shoulder blades together behind you
- Hold for 5 seconds, and then relax
- Repeat 5 to 10 times
- If you are pretty strong and fit, you can do neck rotations while squeezing the shoulder blades
- Remember to keep the shoulders lowered
- Shoulder Rotation
- Rotate one shoulder forwards, alternating left and right sides
- Linda B calls the one shoulder rotation backwards, "Snaggin"
- Pair up to the person next to you and do the shoulder facing them
- Do it 5 to 10 times
- Now pair up with the person on the other side of you and "snag them"
- Again, 5 to 10 times
- Rotate one shoulder forwards, alternating left and right sides
- Rotate one shoulder forwards
- Similar to "snagging" but is called the "Bettie Boop"
- Do in both shoulders at the same time forwards
- This is "shoulders going around the world"
- Repeat 5 - 10 times
- Do both shoulders backwards
- "Superman turning back time"
- Do 5-10 times
- Arm circles
- Position arms straight and out to side (parallel to ground) and proceed to make mini arm circles 10 forward motion and 10 backwards.
- Michael Phelps stretch
- While standing or sitting on a stool (no back support) make a hugging motion with movement with goal of touching your own back with hands. 10 repetitions.
- Wall slides
- While facing a straight wall with staggered stance (one foot touching wall) position arms so that both hands and elbows are touching the wall
- The goal of the exercise will be to raise arms along wall vertically maintaining both hand and elbow contact the entire time
- As you progress higher when elbow loses contact with the wall bring arms back and squeeze (retract shoulder blades) and place arms back at starting position
- Repeat exercise 10 times aiming to increase vertical distance with wall contact.
- Half kneeling 2 way rotation
- From half kneeling position, place hands on inside of knee that is up on the floor
- Rotate body with arm extended to each side reaching for the ceiling and maintaining eye contact with hand throughout motion
- Repeat 5 times each way on one side then switch kneeling leg and repeat on other 5 times.
- Child’s pose to back extension
- From full kneeling position with hands on floor, lower head to ground while sliding hands along floor and pushing shoulders “away from body”
- Return to starting position and with hands on floor arch back pushing chest out and retract shoulder blades
- Repeat 5 times each
Upper body exercises (weighted and non weighted)
- Shoulder shrug
- Shrug (lift and squeeze the shoulders up toward your ears) and breathe in
- Lower the shoulders slowly and exhale
- Linda B calls the shoulder shrug, the "don't know" (inhale) and "oh well" (exhale)
- Fist clenches
- Squeeze fists for 3 seconds, and then relax for 3 seconds
- You can do this one in different positions, depending on how strong and flexible you are (and of course with the therapists or providers "okay")
- The positions may include (standing straight up with good posture of course):
- Fists by your hips (you may grip all your fingers at the same time, or roll them in little finger in first, then ring finger, and so on)
- Fists waist high in front of your body (keep shoulders down and relaxed)
- Fists shoulder height in front of your body (very carefully, especially if you have not healed from your surgery) "grip the staff from the healer" and "release the staff to the healer
- Fists shoulder height out to the sides of your body - keeping shoulders lowered and loose/relaxed (only do this if you have healed from your surgery)
- You can do this one rotating your wrists so that your fists are upright (vertical) or parallel with mother earth (horizontal)
- Horizontal with palms downward = "Dropping the chicken feed"
- You can rotate to the four directions doing this one (and several of the earlier ones too)
- "Offering the corn pollen" is horizontal with palms facing the sky
- Fists above your neck or head - only if therapist and provider approve and your skin and body are healed from your surgery
- Slowly and gently raise the arms as high as is comfortable for you
- You may need to keep your arms bent
- That is fine
- You may need to keep your arms bent
- Keep it comfortable so that you are not hurting yourself
- Fists closed, the open to welcome the blessings from the Creator
- "Thank you, Creator for another good day"
- You can do this one with arms in front of your body or to the sides of your body
- Slowly and gently raise the arms as high as is comfortable for you
- As your body gets stronger, you can combine some of these
- Like hold the bucket with chicken feed with the left arm, reach in with the right to feed the chickens
- Always using slow and gentle movements
- Like hold the bucket with chicken feed with the left arm, reach in with the right to feed the chickens
- Shoulder touch
- Make a fist with the right hand and touch it to the chest, or if you are stronger and more flexible, touch it to your left shoulder
- This is the "I promise"
- You can make private promises or out loud promises
- "I promise to do something good today for my community"
- "I promise to do something good today for my family"
- "I promise to do something good today for myself"
- You can quietly decide what that "something" is to be
- Then do this with the left hand in a fist and touch your left chest or shoulder. "Put on the back pack." Repeat 5 to 10 times
- Berry picking
- Stretch out arm and lean forward (bend your knees a little)
- Clench your fist and bring to your mouth
- Return your empty hand to your side
- Stretch our arm and lean forward again (bend your knees a little)
- Clench your fist and bring to your shoulder put the berries in your gathering sack to bring some berries back to the family
- Repeat 5 to 10 times
- Then do the same movements using the other arm and fist
- Stretch out arm and lean forward (bend your knees a little)
- Spider Woman
- Stand (or sit) in front of the wall
- Let your fingers slowing climb like a spider up the wall, then down
- When you feel strong, Spider Woman can weave a web on the wall
- Start with small circles for the beginning of her web and the circles gradually get larger and larger
- Do this one hand at a time
- Climb from one world to the next
- Kokopelli leads the way from the inner world up to the next world
- Raven leads from out of the home in Mother Earth to above the ground
- You slowly reach up to grab the imaginary ladder rung with one arm and hand to pull yourself up
- Repeat with the other arm and hand of pull yourself up
- Move through the bushes or swimming breast stroke
- Bring both arms forward with palms together as pointing your way through dense brush and bushes
- Slowly turn the palms outward and pull the arms around to the side (to push the bushes aside so that you can move forward)
- Lower your hands to your sides
- Twist the apple stem or light bulb change
- Raise your arm above your head
- Rotate your hand as if screwing in a light bulb or twisting the apple (or apple stem) from the tree limb
- Do with your other arm and hand
- 5 -10 sides on each side
- Finger dexterity
- Place palms and fingers together
- Pull the thumbs toward your chest then back to your palms
- Then pull the index fingers toward your chest and back to the original position
- Then the "live long and prosper" position and back to the original position
- Then from the ring finger and the rest of the hand toward the chest and back to the original position
- Last, do from the little finger and rotate whole praying hands to the chest and back to the original position
- Finger coordination
- Open both palms facing skyward
- Start with right hand and touch right thumb of palm of left open hand
- Return to original open palm position
- Next, move right index finger to touch middle finger of left hand
- Return to original open pal position
- Then move right little finger to touch left index finger
- Repeat with the opposite hands and fingers
- You can change which fingers you touch and use, but try to include all 10 at same time in the activity
- Hold a ball in your lap and squeeze the ball with both hands
- Hold for 3 seconds and then relax
- Repeat 5 to 10 times
- Roll the ball along your waist
- Using both hands hold the ball at your waist and roll the ball to your left side (waist height)
- Keep your shoulders low and relaxed
- Then slowly roll the ball to your right side (keeping in waist height throughout the roll)
- Roll the ball on your thigh
- Sitting down and using both hands, roll the ball length-wise down your thigh, then back up
- Do this on both legs about 5 to 10 times
- Roll the ball around your thigh
- Move your bottom to the front of the chair
- Then using one hand roll the ball under your thigh and with the other hand continue rolling the ball back on top of your thigh (try to not drop the ball
- Do this about 5 to 10 times
- Then repeat the activity with the other thigh
- Move your bottom to the front of the chair
- Push ups (elevated).
- Using a wall or elevated structure, with feet on ground shoulder with, slowly lower chest to structure maintaining 45 degree elbow position (do not let elbows flare out to 90 degrees).
- Lower until hands are parallel with chest (sternum)
- Press through palms and return to starting position
- Repeat 8-12 times
- Can be progressed by lowering structure to a more parallel push up and less elevated with hands
- Canned food upper body exercises
- You may use different sizes and weights of cans depending on how strong you feel
- Hold the can of food (whatever weight you are comfortable with - so you may start out with a can of soup, then later with a large can of tomatoes)
- Or you may find it easier to use a light, but larger container, like the oatmeal carton
- Sit if you are more comfortable
- Stand if you feel strong
- Hold your elbows firmly against the side of your body
- Hold the can of food so that it is parallel with the ground and you are holding the round ends of the can or object
- Slowly curl the object towards your chest keeping your elbows against your sides (don't let your elbows move with the activity), then lower to waist height
- Repeat 5-10 times
- With provider's permission, do more repetitions as you feel stronger and stronger, or increase the weight of the object you are using
- Using two cans
- If the arm that has had lymphedema is weaker, use a lower weight can in that hand
- Stack one can on top of the other
- Hold the higher of the two cans in the position in front of you, then stack the other can on top of it
- Again hold the higher can in the same position and stack the other can on top of it
- When you feel stronger and with the permission of your provider or therapist, you can use a longer object to get more movement
- You can be creative in what you choose to use for the longer object
- It may be a staff, a broom, an arrow, a flute, a pipe, or any other object you feel comfortable holding and moving
- Hold the long object vertically (sitting or standing) and walk your hands on top of one another to climb to the top of the object and then down to the bottom of the object
- "Fatter" objects (like the flute) use fingers differently than tinier objects (like the arrow)
- Hold the long object in the middle with both hands about 6 inches apart
- Rotate the long object alternately like a kayak paddle
- You can also use a rolled up towel (length wise) for this activity
- Pull the towel taunt so that it is stretched out
- Now just rotate it like a figure 8 directly in front of your body
- Then pull the lower part as though you are paddling through water
- Body rotation
- Hold the long object close to its ends out in front of you so that it is parallel with the ground
- Slowly turn your body with the object to the right hold the position for 3 to 5 seconds, then rotate to the left, again, hold the position for 3 to 5 seconds
- Stand and Balance
- When you are feeling very strong and have good balance, stand up leaning on the wall (to help prevent you from falling down) and do the same activity standing up on one leg with the other leg and knee bent
- Plank
- Plant hands directly under shoulders (slightly wider than shoulder width)
- Ground toes into the floor and squeeze glutes to stabilize your body
- Maintain proper spine alignment by slightly tilting hips back (up)
- Hold position while controlling breathing 20 seconds and progress if rpe is low
- Hollow hold
- Lay flat on your back with hands placed on ground to side for support
- While pointing toes down, lift legs 6 inches off floor and hold position for 20 seconds bracing core
Dynamic warm up exercises “lower body”
- NOTE: Remember to wear your leg sleeve(s) before you do any of these exercises and have your provider or therapist tell you which ones are okay for you to do
- Side leg kicks
- From standing position facing wall (or using chair), position both hands on wall for support. Proceed to do side leg swings outwardly 10 on each side. Keep foot flat through motion.
- Hip openers
- Using wall (or chair) for support, from standing position facing sideways, with outside leg raise knee and move in outward circle and return to starting position. Perform 10 on each leg moving front to back.
- Reverse lunge and sky reach.
- From standing position step back on one leg bending knee and with both hands reach towards sky. Exercise can be progressed from a step back (limited knee bend) to full lunge based on individual. Repeat 5 each side
- Leg crossovers
- Lying on your back with your arms outstretched in a “T” formation, bring your right leg across your body so that our toes meet your left hand
- Return to start and repeat with left leg
- Go for 10 reps total
- Prone scorpions
- While laying on stomachs in “T” formation face toward the floor, roll your body to the left so that your right heel comes across your body to meet your left hand
- Return to starting position
- Repeat 5 each side
Lower body exercises (weighted and non weighted)
- Box squats
- Using a chair while sitting down with feet slightly wider than shoulder with, proceed to stand up while pressing through heels and keeping shoulders retracted and chest pressed out
- Head should be in neutral position facing forward
- Repeat 8-12 times while focusing on controlling movement
- Exercise can be progressed from sitting down completely on each repetition, to tapping butt on chair and standing not sitting down completely
- Side walks
- From standing position with slight knee bend take lateral step to widen stance with outside leg and follow by moving inside leg in same direction
- Repeat 10 times consecutively then switch directions, but maintain whatever way you were facing
- Exercise can be progressed to resistance bands around shins with ok from health practitioner
- Sit in a chair and place a dry wash cloth on the floor
- Use bare feet, one at a time to move the toes to gather the wash cloth into a ball or bunch
- Try to grip the wash cloth with your toes and lift it off the ground about 3 inches
- Do the same activity with the other bare foot
- Place small ball (like a foam ball or tennis ball) on the floor and sit in the chair.
- With bare feet using one foot at a time, roll the ball forward, then back towards the chair
- Then roll the ball to the right, and back towards the chair
- Then to the left and back towards the chair
- When you feel strong, do the same activity with your hands holding the chair close to your knees and tuck your chin to your chest
- Use both feet to roll the ball
- Sit in a hard solid chair (not a soft cushion) and tuck your chin to your chest
- Slowly and gently lift the right foot up and straight in front of your body
- Slowly lower the foot to the ground
- Do 5 to 10 times
- Next do the same activity with the left foot
- Do the next activity using different objects, like a pillow, a bath towel rolled up, or a small container of sealed oat cereal
- Sit in a hard solid chair and tuck your chin to your chest
- Place a light object between your knees
- Slowly raise your knees and the object upward and hold the position 3-5 seconds
- Then lower your knees and the object to the ground
- Place a solid chair in front of you, and then lie on your back in front of the chair so that your calves rest on the seat of the chair
- Place the palms of your hands flat on the floor next to your hips
- Raise your head so that your chin is close to your chest
- Try to straighten the right leg up in the air (or in a position that is comfortable for you)
- Lower the leg back to the resting position in the chair
- Do 5 to 10 times
- Then do the same activity with the left leg
- If you are very strong and your provider or therapist says it is okay to do, do the same activity with both legs at the same time
- You must keep your chin tucked close to your chest to help protect your low back from straining
- Lying on your back with the knees bent and your feet flat on the floor
- Place the palms of your hands flat on the floor next to your hips
- Lift your head so that your chin is close to your chest
- Slowly and gently straighten your right leg out so that your foot is a few inches above the floor
- Hold in that position for 3 to 5 seconds
- Bend your knee and lower the foot flat on the floor
- If you feel strong, you can try putting your foot at different heights from the floor
- Do the activity with both legs (check with provider or therapists first please)
- If you feel very strong, you can try to do both legs at the same time
- But check with your provider or therapist before you try to do this